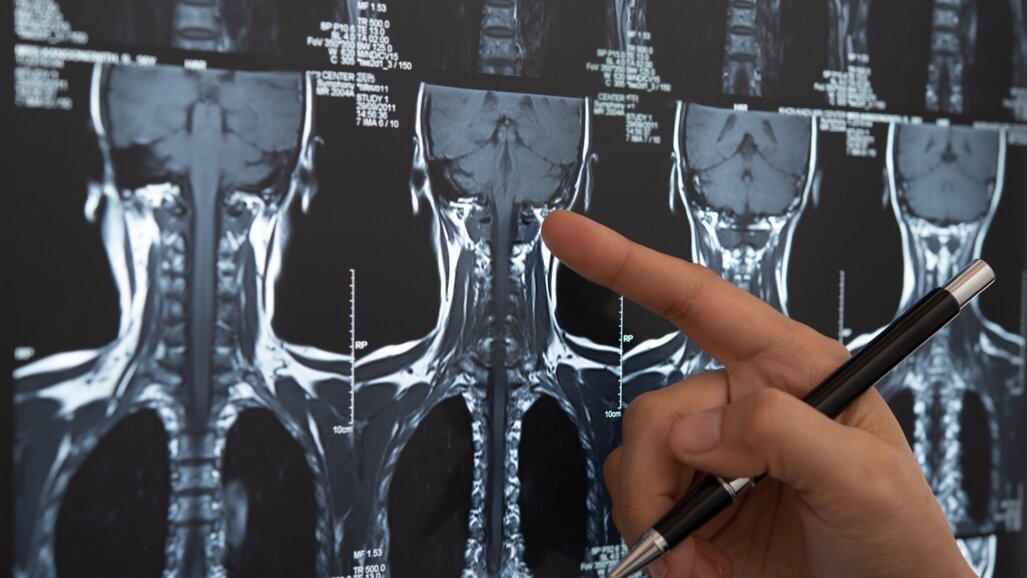
OSLO, Norway: Head and neck cancer is the seventh-most diagnosed cancer group globally, and among its treatment modalities is radiotherapy, used as the primary therapy, as an adjuvant or palliatively. The treatment of head and neck cancer with radiotherapy presents a range of issues for the dental health of patients due to radiation injury to the surrounding normal tissue. A key means of expediting a return to regular oral function has been through the use of dental implants, though the question of whether to place these before or after radiotherapy has been debated. Recent PhD research from the University of Oslo has systematically explored the issue, yielding some highly significant results.
Oral impacts of head and neck cancer treatment
As confirmed by recent scientific research, the implications of head and neck cancer treatment for oral health are numerous and varied. Firstly, what comes as a great shock to many patients is that they may require extraction of teeth with poor prognoses before radiotherapy in order to minimise extraction after therapy, because of the lifelong risk of osteoradionecrosis. Once patients receive radiation to the affected areas, many may experience oral mucositis, fungal infections and loss of taste. Other possible consequences of radiotherapy are reduction of saliva production, leading to caries; tissue fibrosis, causing trismus and pharyngo-oesophageal stenosis; and thin and hypersensitive mucosa, making it uncomfortable to wear removable dental prostheses. An important corollary of these painful and debilitating physiological effects is that patients understandably experience a reduced quality of life, significant emotional difficulties and social impacts.
Implants as a way to restore oral function
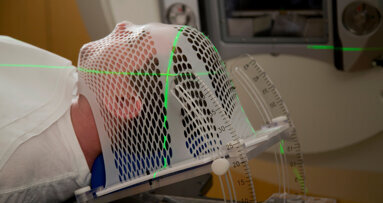
The role of osseointegrated implants in restoring oral function among head and neck cancer patients is well established. However, as Dr Lisa Printzell describes in her recently completed PhD thesis, the use of implants in patients who have undergone or are to undergo radiotherapy presents a range of challenges, mainly related to the reduced ability of irradiated soft tissue and bone to heal. In news on the university’s website, Dr Printzell stated: “The survival of dental implants placed in irradiated jawbone is significantly lower than those placed in non-irradiated patients.”
To circumvent this issue, an increasingly used strategy has been to place implants before radiation has been applied to the head and neck region, giving osseointegration a head start and improving patients’ quality of life sooner through final prosthetic restorations. However, Dr Printzell’s research shows that this approach is not without its shortcomings, particularly the concern of back scatter of radiation by titanium implants, reflecting it on to surrounding tissue and subsequently intensifying the damaging effects of radiotherapy. “When ionising radiation is directed at a cancerous tumour and there is a titanium implant in the radiation field, not all the radiation will penetrate the metal. Instead, it will reflect back to the surrounding tissue,” she explained.
Understanding back scatter better
In order to determine whether back scatter from titanium is of greater threat to osseointegration than the impaired healing capacity of previously irradiated bone, a key part of Dr Printzell’s research has been to systematically explore the effect of back scatter upon two of the most important cell types for bone healing and osseointegration of implants, namely, mesenchymal stem cells and osteoblasts. Using a variety of radiation doses, ranging from 2 Gy to 10 Gy, Dr Printzell measured the extent of the effect of back scatter upon these cell types.
Her results were highly revealing: “We also found that the highest dose of 10 Gy inhibited both cell types’ ability to move from one place to another on titanium, while lower doses (2 and 6 Gy) neither caused significant DNA damage nor affected the cells’ ability to move. The results indicate that back scatter radiation from titanium at doses of 2 Gy does not cause greater cell damage than the same dose does without an implant present.” Such findings thus cast light upon the crucial issue of whether or not it is effective and safe to place implants in head and neck cancer patients before they undergo radiotherapy.
Editorial note:
Dr Lisa Printzell’s thesis, titled The Impact of Radiation Backscatter on Cells Involved in the Osseointegration of Titanium Dental Implants, is available here.
Topics:
Tags:
BARI, Italy: An increasing number of products are appearing on the market aimed at replacing toothpastes and mouthrinses containing synthetic constituents ...
CHAPEL HILL, N.C., US: Head and neck squamous cell carcinoma (HNSCC) is a global health concern, ranking as the sixth most common malignancy worldwide. Poor...
Head and neck cancer may have drastic, long-lasting consequences, and dental professionals can play a crucial role in the patient’s treatment plan. Dental...
As cancer treatments evolve, clinicians of all disciplines must also adapt their approaches to medical and dental treatments in order to best compensate for...
Live webinar
Tuesday, 24. February 2026
19:00 CET (Oslo)
Prof. Dr. Markus B. Hürzeler
Live webinar
Tuesday, 24. February 2026
21:00 CET (Oslo)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wednesday, 25. February 2026
17:00 CET (Oslo)
Prof. Dr. Daniel Edelhoff
Live webinar
Wednesday, 25. February 2026
19:00 CET (Oslo)
Live webinar
Thursday, 26. February 2026
02:00 CET (Oslo)
Live webinar
Tuesday, 3. March 2026
17:00 CET (Oslo)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Wednesday, 4. March 2026
02:00 CET (Oslo)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East



































To post a reply please login or register