As cancer treatments evolve, clinicians of all disciplines must also adapt their approaches to medical and dental treatments in order to best compensate for the powerful side effects of more robust treatment options. Dr Josiane Almeida, researcher and lecturer in the Department of Endodontics at the University of Southern Santa Catarina and Federal University of Santa Catarina in Brazil, will explain to attendees at the 2024 ROOTS SUMMIT how they can best adapt their approaches for patients who have undergone head and neck radiotherapy.
The number of patients treated with radiation therapy is growing as a result of improvements in surgery and radiotherapy techniques. This means more endodontists will be required to be part of a team providing multidisciplinary treatment. Based on your experience, what should clinicians know about endodontic treatments before and after radiotherapy in order to manage the oral health of a patient?
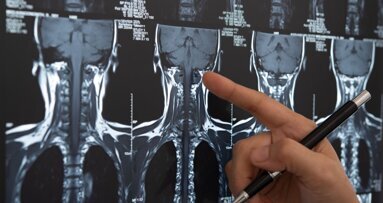
Head and neck cancer poses a significant health challenge on a global scale. Although radiation therapy is highly recommended for cancer treatment, it may produce adverse effects on the patient’s oral condition. The high risk of osteoradionecrosis after radiotherapy limits tooth extraction. Therefore, endodontic treatment is a feasible option for managing oral health. Although an effective root canal treatment avoids serious complications to the patient’s oral health, it is necessary to know how to perform it and the ideal moment to choose, taking into consideration all the concerns that arise as a result of irradiation.
What are some of the specific implications of radiotherapy on endodontic treatment? Do endodontists have to change their treatment procedures in order to treat previously irradiated areas?
The dental structure most affected by radiotherapy is dentine, owing to its high organic content. Some of the alterations are caused by a process called radiolysis, leading to dehydration of the substrate, breakdown of the odontoblastic extensions and collagen fibrils, and cracks and fissures around the dentinal tubules. These alterations make the dental structure more susceptible to fracture and increase the dentinal roughness, which in turn affects the interaction between the substrate and microorganisms. Therefore, microbial colonisation, followed by the establishment of a more complex and structured biofilm, may occur. Bearing this in mind, endodontists need to redirect their treatment procedures regarding patients who have undergone radiotherapy in order to achieve endodontic success and restore oral health.
There seems to be a debate about whether root canal therapy or tooth extraction is the preferred option for patients after radiotherapy. From your clinical experience, what is your opinion on this topic?
The ideal course of action for treating a patient who has been exposed to radiation should involve a collaborative effort between medical and dental professionals. The treatment plan should be well thought out, taking into account all potential risks to the patient. It is clear that tooth extraction in radiation-exposed patients may lead to osteonecrosis and other complications that might harm the patient’s health. For this reason, endodontic treatment is often the preferred option. Nonetheless, the top priority should always be the patient’s overall well-being.
In your presentation, you will speak about future treatment options for patients after radiotherapy. Could you give a preview of what this will entail?
There is limited literature available on the combination of endodontics and radiotherapy. We will not focus on new treatment techniques, as in this sense endodontics itself is already quite advanced, but rather on the damage and structural changes that radiotherapy causes to the dental structures. Additional topics include the way in which such damage can be overcome and the ideal time frame in which to perform endodontics in order to obtain a more effective endodontic treatment with a greater chance of success.
What will be the three main learning objectives of your session at ROOTS SUMMIT 2024?
The objectives will be to address the alterations to dental structures caused by irradiation, to examine irradiation’s impact on endodontic therapy and to discuss appropriate treatment approaches for the affected teeth.
What are you personally looking forward to at next year’s ROOTS SUMMIT?
The event has been successful since its inception. Although I have never before attended in person, I have followed the entire event—speakers, topics covered and excellent organisation—online. I am excited about participating actively this time in Athens and joining the team of speakers. I am confident that the event will provide valuable knowledge for all attendees, as well as an opportunity to network and share experiences.
Editorial note:
Dr Josiane Almeida will be giving a lecture titled “Effect of radiotherapy on dental structures: Current clinic and future treatment perspectives” at the 2024 ROOTS SUMMIT on 11 May 2024 from 11:00 a.m. to 12:30 p.m.
More information on the programme and registration can be found on the ROOTS SUMMIT website.
Tags:
OSLO, Norway: Head and neck cancer is the seventh-most diagnosed cancer group globally, and among its treatment modalities is radiotherapy, used as the ...
AARHUS, Denmark: As the implementation of artificial intelligence (AI) in the dental industry continues to accelerate, there appears to be a growing ...
COPENHAGEN, Denmark: 3Shape, a market-leading provider of digital dentistry and 3D-scanning software, has launched TRIOS Share, a solution that enables ...
KUOPIO, Finland: The dynamics of a visit to the dentist extend far beyond the purely technical elements. The psychological comfort of the patient and the ...
OULU, Finland: Dental fear is one of the most common fears in developed countries. Globally, the overall prevalence in children and adolescents is estimated...
HELSINKI, Finland: Human papillomavirus (HPV) causes roughly 2% of oral cavity or laryngeal cancers and 31% of oropharyngeal cancers, according to a Lancet ...
OSLO, Norway: The painful condition of burning mouth syndrome (BMS) has similar symptoms, including a tingling sensation in the mouth, to conditions such as...
GOTHENBURG, Sweden: In Sweden, free dental check-ups are provided for children and adolescents until they reach the age of 20. Whereas this means that much ...
In June, Dental Tribune International reported on an incisive study that explored the perspectives of dental patients on the ever-increasing role played by ...
MALMÖ, Sweden: As a follow-up to last year’s clinical symposium, which was the first of its kind for TePe, the Swedish oral health company is hosting a ...
Live webinar
Tuesday, 24. February 2026
19:00 CET (Oslo)
Prof. Dr. Markus B. Hürzeler
Live webinar
Tuesday, 24. February 2026
21:00 CET (Oslo)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wednesday, 25. February 2026
17:00 CET (Oslo)
Prof. Dr. Daniel Edelhoff
Live webinar
Wednesday, 25. February 2026
19:00 CET (Oslo)
Live webinar
Thursday, 26. February 2026
02:00 CET (Oslo)
Live webinar
Tuesday, 3. March 2026
17:00 CET (Oslo)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Wednesday, 4. March 2026
02:00 CET (Oslo)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East











































To post a reply please login or register